NCP | Nursing Care Plan Liver Cirrhosis
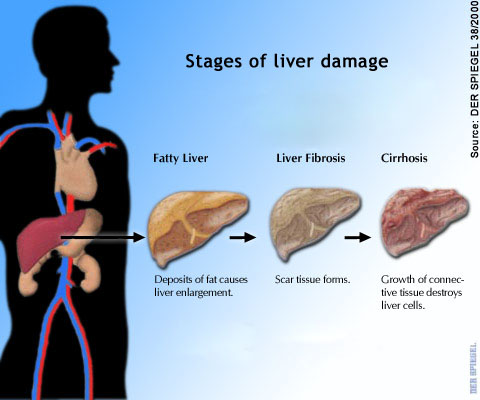
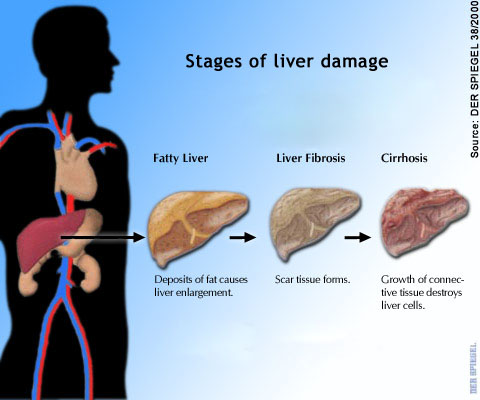
Cirrhosis is a chronic liver disease that is characterized by destruction of the functional liver cells, which leads to cellular death. Cirrhosis along with other chronic liver diseases result in up to 35,000 deaths each year in the United States and is the ninth leading cause of death. In cirrhosis , the damaged liver cells regenerate as fibrotic areas instead of functional cells, causing alterations in liver structure, function, blood circulation, and lymph damage. The major cellular changes include irreversible chronic injury of the functional liver tissue and the formation of regenerative nodules. These changes result in liver cell necrosis, collapse of liver support networks, distortion of the vascular bed, and nodular regeneration of the remaining liver cells. The classification of cirrhosis is controversial at present. However, most types may be classified by a mixture of causes and cellular changes, defined as follows: alcoholic; cryptogenic and postviral or postnecrotic; biliary; cardiac; metabolic, inherited, and drug-related; and miscellaneous. The first three types are the most commonly seen, accounting for 55% to 90% of cases of cirrhosis. Although each of these types has a different etiology, the clinical findings, including portal vein hypertension and eventual liver failure, are much the same
 Liver cirrhosis is most commonly associated with hepatitis C (26% of the cases) alcohol abuse (21%), hepatitis C plus alcohol abuse (15%), cryptogenic causes (etiology not determined; 18%), hepatitis B (15%), and other miscellaneous causes (5%) such as malnutrition, protein deficiency, biliary disease, and chemical toxins. Alcoholic liver disease is also known as Laennec’s, portal, nutritional, and fatty cirrhosis.
Liver cirrhosis is most commonly associated with hepatitis C (26% of the cases) alcohol abuse (21%), hepatitis C plus alcohol abuse (15%), cryptogenic causes (etiology not determined; 18%), hepatitis B (15%), and other miscellaneous causes (5%) such as malnutrition, protein deficiency, biliary disease, and chemical toxins. Alcoholic liver disease is also known as Laennec’s, portal, nutritional, and fatty cirrhosis.
Nursing care plan liver cirrhosis physical assessment and examination
Determine if the patient has experienced personality changes such as agitation, forgetfulness, and disorientation. Inquire about fatigue, drowsiness, mild tremors, or flulike symptoms. Ask about any past or present symptoms that may indicate cirrhosis, such as changes in bowel habits or menstrual irregularities. Elicit a history of easy bruising, nosebleeds, or bleeding gums. Determine the patient’s drinking patterns and how long they have existed. Determine if the patient has had early-morning nausea and vomiting, anorexia, indigestion, weight loss, weakness, lethargy, epigastric discomfort, or altered bowel habits. Ask about any recent sexual dysfunction.
Inspect for signs of muscle atrophy. Note whether the patient’s abdomen is protruding. Assess the patient’s skin, sclera, and mucous membranes, observing for poor skin turgor, signs of jaundice, bruising, spider angiomas, and palmar erythema (reddened palms). Observe the patient’s trunk, and note the presence of gynecomastia (enlarged breasts). Observe the abdomen for distension, an everted umbilicus, and caput medusae (a plexus of dilated veins about the umbilicus); measure the abdominal girth. When assessing the patient’s upper extremities, test for asterixis (liver flap or flapping tremor). Have the patient stretch out her or his arm and hyperextend the wrist with the fingers separated, relaxed, and extended. The patient in stages II (impending) and III (stuperous) of hepatic encephalopathy may have a rapid, irregular flexion and extension (flapping) of the wrist. Note any tenderness or discomfort in the patient’s abdomen. Palpate for hepatomegaly by gently rolling the fingers under the right costal margin. The liver is normally soft and usually can be felt under the costal margin. Percuss the patient’s abdomen. Note a shifting dullness in the abdomen if ascites is present. Auscultate the abdomen and assess for hypoactive, hyperactive, or normal bowel sounds.
Cirrhosis is a chronic disease that dictates lifestyle changes for the patient and significant others. Determine the patient’s response to the diagnosis and his or her ability to cope with change. Identify the patient’s past ability to cope with stressors, and determine if these mechanisms were successful.
Nursing care plan liver cirrhosis with a primary nursing diagnosis of Fluid volume excess related to retention.
Nursing care plan liver cirrhosis intervention and treatment plan
Patients are placed on a well-balanced, high-calorie (2500 to 3000 calories per day), moderate- to high-protein (75 g of high-quality protein per day), low-fat, low-sodium diet (200 to 1000 mg per day), with additional vitamins and folic acid. Accurate fluid intake and output are important to prevent fluid volume overload; for most patients, intake should be limited to 500 to 1000 mL per day. Frequently, vitamin K injections are ordered to improve blood clotting factors. If coagulopathies worsen, treatment may require whole blood or fresh-frozen plasma to maintain the hematocrit and hemoglobin. If alcohol is the primary etiologic factor in liver cirrhosis, strongly encourage the patient to cease drinking.
Surgical intervention includes a LaVeen continuous peritoneal jugular shunt (peritoneovenous shunt), which may be inserted for intractable ascites. This procedure allows the continuous shunting of ascitic fluid from the abdominal cavity through a one-way valve into a silicone tube that empties into the superior vena cava. Paracentesis may be performed if conditions warrant. Indicators include a large volume of ascitic fluid that compromises the patient’s respirations, causes abdominal discomfort, or poses a threat of rupturing an umbilical hernia.
Commonly seen in cirrhosis patients are esophageal varices due to portal vein hypertension. Varices can rupture as a result of anything that increases the abdominal venous pressure, such as coughing, sneezing, vomiting, or the Valsalva’s maneuver. To remedy bleeding of esophageal varices, a Sengstaken-Blakemore tube can be placed. In cases of irreversible chronic liver disease, liver transplantation is an option; however, there are selection criteria. Candidates for liver transplantation fall into three categories: those with irreversible chronic liver disease; those with malignancies of the liver and biliary tree; and those with fulminant hepatic failure. Liver transplantation is considered an important therapeutic option for patients with end-stage liver disease, with 1-year and 5-year survival rates of 70% and 60%, respectively.
Nursing considerations in the cirrhotic patient are to avoid infection and circulatory problems. Turn the patient and encourage coughing and deep breathing every 2 hours to prevent pneumonia.
Because bleeding can occur, monitor the patient closely for signs of hypovolemia. Test any stool and emesis for blood. Follow closely any break in the patient’s skin integrity for increased bleeding, and apply pressure to injection sites. Warn the patient against straining at stool, blowing her or his nose, or sneezing too vigorously. Suggest the patient use a soft toothbrush and an electric razor. Because of fatigue, muscle atrophy, and wasting, the patient needs to rest. Plan activities to include regular rest periods. To prevent breakdown of the skin, place the patient on an egg-crate or air mattress. Avoid using soap to bathe the patient; use moisturizing agents or lubricating lotion. Use pressure-reducing mattresses or specialty beds to prevent skin breakdown. Apply lotion and massage areas of the skin that are potential breakdown sites.
Encourage the patient to verbalize questions, anxieties, and fears. In conversation, note any behavioral or personality changes, including increasing stupor, lethargy, or hallucinations. Arouse the patient periodically to determine his or her level of consciousness. Emotional and psychological support for the patient and family are important to eliminate anxiety and poor self-esteem. Involve the family members in the patient’s care as a means of improving the patient’s morale.
Nursing care plan discharge and home health care guidelines
Emphasize to the patient with alcoholic liver cirrhosis that continued alcohol use exacerbates the disease. Stress that alcoholic liver disease in its early stages is reversible when the patient abstains from alcohol. Encourage family involvement in alcohol abuse treatment. Assist the patient in obtaining counseling or support for her or his alcoholism. Encourage the patient to seek frequent medical follow-up. Visits from a community health nurse to monitor the patient’s progress and to help with any questions or problems at home are also helpful. Refer the patient to an alcohol support group or liver transplant support group.
Nursing care plan liver cirrhosis physical assessment and examination
Determine if the patient has experienced personality changes such as agitation, forgetfulness, and disorientation. Inquire about fatigue, drowsiness, mild tremors, or flulike symptoms. Ask about any past or present symptoms that may indicate cirrhosis, such as changes in bowel habits or menstrual irregularities. Elicit a history of easy bruising, nosebleeds, or bleeding gums. Determine the patient’s drinking patterns and how long they have existed. Determine if the patient has had early-morning nausea and vomiting, anorexia, indigestion, weight loss, weakness, lethargy, epigastric discomfort, or altered bowel habits. Ask about any recent sexual dysfunction.
Inspect for signs of muscle atrophy. Note whether the patient’s abdomen is protruding. Assess the patient’s skin, sclera, and mucous membranes, observing for poor skin turgor, signs of jaundice, bruising, spider angiomas, and palmar erythema (reddened palms). Observe the patient’s trunk, and note the presence of gynecomastia (enlarged breasts). Observe the abdomen for distension, an everted umbilicus, and caput medusae (a plexus of dilated veins about the umbilicus); measure the abdominal girth. When assessing the patient’s upper extremities, test for asterixis (liver flap or flapping tremor). Have the patient stretch out her or his arm and hyperextend the wrist with the fingers separated, relaxed, and extended. The patient in stages II (impending) and III (stuperous) of hepatic encephalopathy may have a rapid, irregular flexion and extension (flapping) of the wrist. Note any tenderness or discomfort in the patient’s abdomen. Palpate for hepatomegaly by gently rolling the fingers under the right costal margin. The liver is normally soft and usually can be felt under the costal margin. Percuss the patient’s abdomen. Note a shifting dullness in the abdomen if ascites is present. Auscultate the abdomen and assess for hypoactive, hyperactive, or normal bowel sounds.
Cirrhosis is a chronic disease that dictates lifestyle changes for the patient and significant others. Determine the patient’s response to the diagnosis and his or her ability to cope with change. Identify the patient’s past ability to cope with stressors, and determine if these mechanisms were successful.
Nursing care plan liver cirrhosis with a primary nursing diagnosis of Fluid volume excess related to retention.
Nursing care plan liver cirrhosis intervention and treatment plan
Patients are placed on a well-balanced, high-calorie (2500 to 3000 calories per day), moderate- to high-protein (75 g of high-quality protein per day), low-fat, low-sodium diet (200 to 1000 mg per day), with additional vitamins and folic acid. Accurate fluid intake and output are important to prevent fluid volume overload; for most patients, intake should be limited to 500 to 1000 mL per day. Frequently, vitamin K injections are ordered to improve blood clotting factors. If coagulopathies worsen, treatment may require whole blood or fresh-frozen plasma to maintain the hematocrit and hemoglobin. If alcohol is the primary etiologic factor in liver cirrhosis, strongly encourage the patient to cease drinking.
Surgical intervention includes a LaVeen continuous peritoneal jugular shunt (peritoneovenous shunt), which may be inserted for intractable ascites. This procedure allows the continuous shunting of ascitic fluid from the abdominal cavity through a one-way valve into a silicone tube that empties into the superior vena cava. Paracentesis may be performed if conditions warrant. Indicators include a large volume of ascitic fluid that compromises the patient’s respirations, causes abdominal discomfort, or poses a threat of rupturing an umbilical hernia.
Commonly seen in cirrhosis patients are esophageal varices due to portal vein hypertension. Varices can rupture as a result of anything that increases the abdominal venous pressure, such as coughing, sneezing, vomiting, or the Valsalva’s maneuver. To remedy bleeding of esophageal varices, a Sengstaken-Blakemore tube can be placed. In cases of irreversible chronic liver disease, liver transplantation is an option; however, there are selection criteria. Candidates for liver transplantation fall into three categories: those with irreversible chronic liver disease; those with malignancies of the liver and biliary tree; and those with fulminant hepatic failure. Liver transplantation is considered an important therapeutic option for patients with end-stage liver disease, with 1-year and 5-year survival rates of 70% and 60%, respectively.
Nursing considerations in the cirrhotic patient are to avoid infection and circulatory problems. Turn the patient and encourage coughing and deep breathing every 2 hours to prevent pneumonia.
Because bleeding can occur, monitor the patient closely for signs of hypovolemia. Test any stool and emesis for blood. Follow closely any break in the patient’s skin integrity for increased bleeding, and apply pressure to injection sites. Warn the patient against straining at stool, blowing her or his nose, or sneezing too vigorously. Suggest the patient use a soft toothbrush and an electric razor. Because of fatigue, muscle atrophy, and wasting, the patient needs to rest. Plan activities to include regular rest periods. To prevent breakdown of the skin, place the patient on an egg-crate or air mattress. Avoid using soap to bathe the patient; use moisturizing agents or lubricating lotion. Use pressure-reducing mattresses or specialty beds to prevent skin breakdown. Apply lotion and massage areas of the skin that are potential breakdown sites.
Encourage the patient to verbalize questions, anxieties, and fears. In conversation, note any behavioral or personality changes, including increasing stupor, lethargy, or hallucinations. Arouse the patient periodically to determine his or her level of consciousness. Emotional and psychological support for the patient and family are important to eliminate anxiety and poor self-esteem. Involve the family members in the patient’s care as a means of improving the patient’s morale.
Nursing care plan discharge and home health care guidelines
Emphasize to the patient with alcoholic liver cirrhosis that continued alcohol use exacerbates the disease. Stress that alcoholic liver disease in its early stages is reversible when the patient abstains from alcohol. Encourage family involvement in alcohol abuse treatment. Assist the patient in obtaining counseling or support for her or his alcoholism. Encourage the patient to seek frequent medical follow-up. Visits from a community health nurse to monitor the patient’s progress and to help with any questions or problems at home are also helpful. Refer the patient to an alcohol support group or liver transplant support group.

1 komentar:
I was diagnosed as HEPATITIS B carrier in 2013 with fibrosis of the
liver already present. I started on antiviral medications which
reduced the viral load initially. After a couple of years the virus
became resistant. I started on HEPATITIS B Herbal treatment from
ULTIMATE LIFE CLINIC (www.ultimatelifeclinic.com) in March, 2020. Their
treatment totally reversed the virus. I did another blood test after
the 6 months long treatment and tested negative to the virus. Amazing
treatment! This treatment is a breakthrough for all HBV carriers.
Posting Komentar